The cure for obesity:
A MUST-SEE: ‘Fat, Sick & Nearly Dead’ (Full Documentary):
100 pounds overweight, loaded up on steroids and suffering from a debilitating autoimmune disease, Joe Cross is at the end of his rope and the end of his hope. In the mirror he saw a 310lb man whose gut was bigger than a beach ball and a path laid out before him that wouldn’t end well- with one foot already in the grave, the other wasn’t far behind. FAT, SICK & NEARLY DEAD is an inspiring film that chronicles Joe’s personal mission to regain his health. With doctors and conventional medicines unable to help long-term, Joe turns to the only option left, the body’s ability to heal itself.
– “Survival Of The Fattest”: It’s A Fat, Fat World After All (ZeroHedge, Nov 24, 2012):
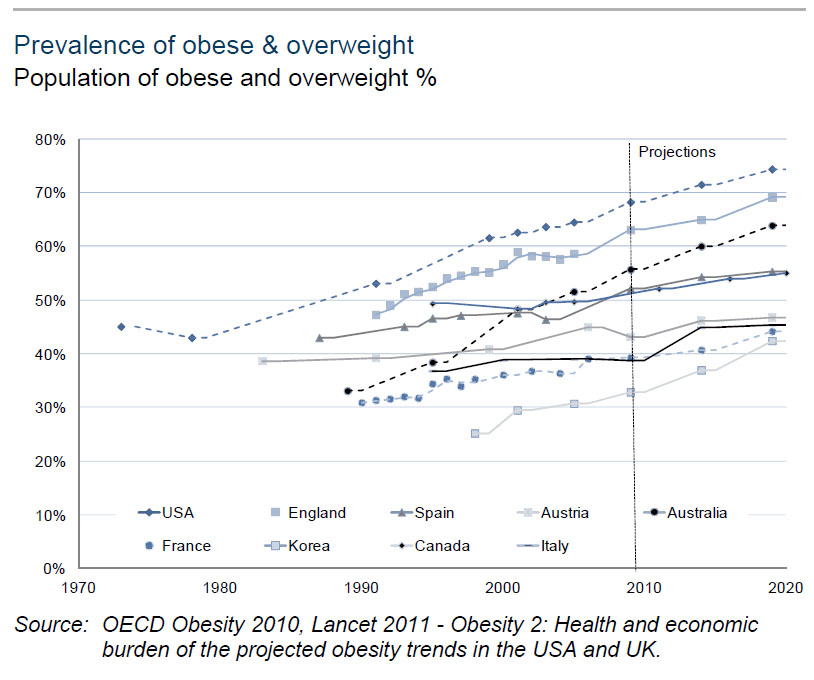
Back in March, we first presented a rather stunning finding: by 2020 75% of Americans will be obese or overweight. This was promptly followed up with a post showing just how it is transpired that America became the fattest nation in the world in less than 20 years. What however may not be known, is that America’s fatness epidemic is not localized to the country that gave the world the McDonalds burger (and the McMansion): it really is a fat, fat world, after all. Behold – survival of the fattest:
It is hardly surprising in this light, then, that the estimate for number of people living with diabetes has been increased, to 371 million – an increase of 11% over 2011.
So with the sensitive issue of what one stuffs in their mouth becoming of paramount importance, primarily due to the avalanche in social costs as a result of escalating morbid obesity, here is a primer on the key facts and figures relating to obesity, domestic as well as foreign, and impacting not just the developed world but also emerging economies, from GS’ Mick Ready and Keyur Parekh.
Obesity is a unique phenomenon affecting almost all countries. It is defined as excessively high amount of body fat in relation to lean tissue, and individuals are generally considered overweight if their BMI is over 25, and clinically obese if their body mass index (BMI) is greater than 30.
The 1980s saw a sharp acceleration in BMI in OECD countries. Before 1980, global obesity rates were generally below 10% but today, in almost half of OECD countries, 50% of the population is overweight. Interestingly, data suggests that obesity is a pandemic that is now impacting not just the developed western countries, but also the emerging economies. In BRIC economies, obesity rates are somewhat lower than in their OECD counterparts, but urbanisation and lifestyle changes are driving a significant increase in average BMI. In China, the proportion of the population considered overweight increased from 13.5% in 1991 to 26.7% in 2006; in Brazil between 1975 and 2003, the obesity rate tripled in men and doubled in women; and in Russia 25% of women and 10% of men are now considered obese.
- Data suggest that at levels of GDP below US$5,000 per capita there is a linear relationship between GDP and mean BMI, and that the only pre-condition for developing an obese population is the ability to afford food.
- In low income countries, obese individuals are typically middle-aged women from wealthy, urban settings.
- In countries with GDP of more than US$5,000 per capita pa, obesity is not characterized by gender, or age, but disadvantaged groups typically are at greater risk of becoming obese;
- 33% of US adults earning over US$15,000 pa are obese, compared with 25% of those earning over US$50,000 pa.
- 33% of adults who did not graduate high school were obese, compared with 21.5% who graduated from college.
What’s causing this increase?
Obesity is a complex problem, with multiple factors influencing its development within a population. These factors include systemic and environmental drivers, which provide an infrastructure to promote high growth, consumption of transport and recreational factors, which limit the physical activity within a population, and behavioral patterns, where individuals consume high-energy foods and lead sedentary lifestyles.
For an individual, obesity is caused by an energy imbalance: simply put, obese individuals consume more energy than they use. Energy intake is a clear factor in the rise of obesity, and dietary intake is strongly influenced by the kinds of food we eat. Changes in the food system to more mass-produced, processed foods with added salt, fats and sugars, coupled with more effective marketing of these products, especially targeting young children has changed the kind of food we eat which contributes to this energy imbalance.
To summarize, changes in the global food system, which produces readily available, inexpensive, highly processed and well marketed foods, coupled with changes in working patterns, has created an energy imbalance resulting in increased levels of obesity.
Sugary drinks: The choice of a heavy generation
There are multiple factors which are linked to the development of obesity globally, but sugar-sweetened drinks have attracted particular attention in the US. Sugar intake from sugar-sweetened drinks is thought to be the largest single caloric food source in the US, approaching 15% of the daily calorific intake in several population groups.
High-sugar drinks are effectively marketed to children and young adults, and their consumption is often linked to fast food, which is likely to exacerbate the obesity problem. Many sugar-sweetened drinks contain high-fructose corn syrup, and there is evidence to suggest a link between high-fructose corn syrup and the development of insulin resistance (think diabetes). Multiple studies have shown that replacing a sugar-containing drink with a sugar-free equivalent significantly reduced weight gain and fat accumulation in normal weight children, prompting calls from the American Heart Association, the Institute of Medicine, and the Obesity society to reduce consumption of sugar-sweetened beverages.
The consequences of being obese: Shorter, less healthy lives The life expectancy of a person with a BMI of 40-45 is reduced by around 8-10 years, which is similar to the reduction in life expectancy suffered by smokers. An overweight person of average height increases their risk of death by around 30% for every 15kg of weight. Obesity is a key risk factor in the development of multiple diseases, including diabetes, heart disease, osteoarthritis and
cancer.The most direct and obvious impact of obesity is on incidence of diabetes – a severely obese person is around 60 times more likely to develop diabetes than someone with normal weight. High blood pressure and high cholesterol levels are also linked to high BMI.
These combined risk factors make an obese individual more likely to die from heart disease or stroke.
But perhaps a less intuitive link is the one between obesity, physical inactivity and cancer. Obesity and physical inactivity are also a key risk factor in the development of certain cancers; around 9% of colorectal cancers, and 11% of postmenopausal breast cancer in women is linked to obesity. An additional 5kg/m2 in BMI is thought to increase the risk of colorectal cancer by 24% in males, and to increase the risk of postmenopausal breast cancer in women by 12%.
Obesity and cancer – the not so obvious link
According to the American Cancer Society, one-third of cancer deaths are linked to obesity and/or lack of physical activity.
Improvements in cancer diagnosis, treatment and prevention has seen an improvement in death rates for cancer in the US over recent years, but the obesity epidemic within the US puts this trend at risk. Obesity is a known risk factor for multiple different tumour types, including oesophageal, colorectal, endometrial, kidney and certain breast cancers. In addition to increasing the risk of developing certain cancers, obese individuals are less likely to survive their cancer diagnosis; individuals with a BMI above 40 had death rates 52% higher for men and 62% higher for women when compared to people of normal weigh.
Obese men are at significantly higher risk of developing colorectal cancer; the distribution of body fat appears to be an important fact, with abdominal obesity measured by waist circumference demonstrating a strong correlation with colon cancer risk. Obesity also modestly increases the risk of women developing postmenopausal breast cancer.
The costs of an obese population – direct, but also indirect Obese populations place greater stress upon healthcare systems already struggling to cope with rising expectation on what healthcare systems can deliver, more expensive medical interventions and an increasingly elderly population. The chronic nature of the condition means that obese people consume a greater share of healthcare resources, over a longer period of time.
Medical costs for obese individuals are as much as 30% to 40% higher than those with normal weight. An obese individual will on average visit a physician 27% more frequently than someone with a normal weight, and the annual extra medical costs of obesity in the US were estimated to be US$75 bn in 2003 (BMJ Wang). If current demographic trends continue, obesity-related costs are set to double every ten years, and could account for 16%-18% of US Healthcare expenditure by 2030. In the UK, data point to a similar trend, with £650 mn increased annual costs by 2020, and £2 bn higher costs by 2030 (Wang).
In addition to the direct medical costs for treating obesity, there are indirect costs to society and economies, which include early retirement and lost or lower productivity. US data suggest a direct correlation between obesity and missed work days in men, with males with a BMI above 40 taking almost six additional sick days each year. Swedish data suggest obese individuals are 1.5-1.9 times more likely to take sick leave than their peers with normal weight.
Who provides the solutions?
Before we get to the investing implication of this pandemic, we believe it’s worth spending a minute on the impact that reversal of current trends might have, and the role that various parties have played thus far to resolve this. Perhaps slightly depressingly, we believe that pharma companies alone are unlikely to be able to resolve this. Indeed we believe that a majority of this change message needs to come from government policy and social change (as we saw in the 1970s-80s with smoking).
What are the benefits if trends reverse?
Modest changes can have a dramatic impact on both an individual’s risk profile and society as a whole. A 1% reduction in BMI (approximately losing 1kg of body weight) is estimated to reduce cases of diabetes by around 2 million, and cases of cancer by around 100. However, implementation of these changes will require behavioural changes through health promotion campaigns and policy interventions to address healthy public sector food service policies. But policy and behavioural changes are not easy to implement and take time to take effect.
Pharma industry response – encouraging, but not adequate
Despite numerous attempts, the pharmaceutical industry has had limited success in addressing the primary cause of obesity (energy imbalance). Current treatments combat the consequences of obesity, e.g., through the management of hypertension, or diabetes.[ZH: perhaps the profit potential is far greater in perpetuating the underlying cause and merely treating the symptoms which have a duration that expires with the expiration of the patient?] A large number of companies have tried to develop pharmaceuticals to target energy imbalance, but the vast majority have failed owing to serious toxic effects. For example, Sanofi’s Accomplia was abandoned for suicidal ideation, Fen-Phen was withdrawn for serious cardiovascular concerns, and sibutramine was recently withdrawn following cardiovascular safety concerns.
2012 has seen the FDA approval of two new treatments for obesity, when used in conjunction with reduced calorie diets. Both Belviq (Arena Pharmaceuticals) and Qsymia (Vivus) reduce appetite and in some people can induce a negative energy balance. Both products have demonstrated safety signals which are a cause for concern, and patients receiving these products will require careful monitoring by clinicians. But, the FDA’s willingness to approve agents with clear safety signals illustrates the need for effective intervention for obesity.
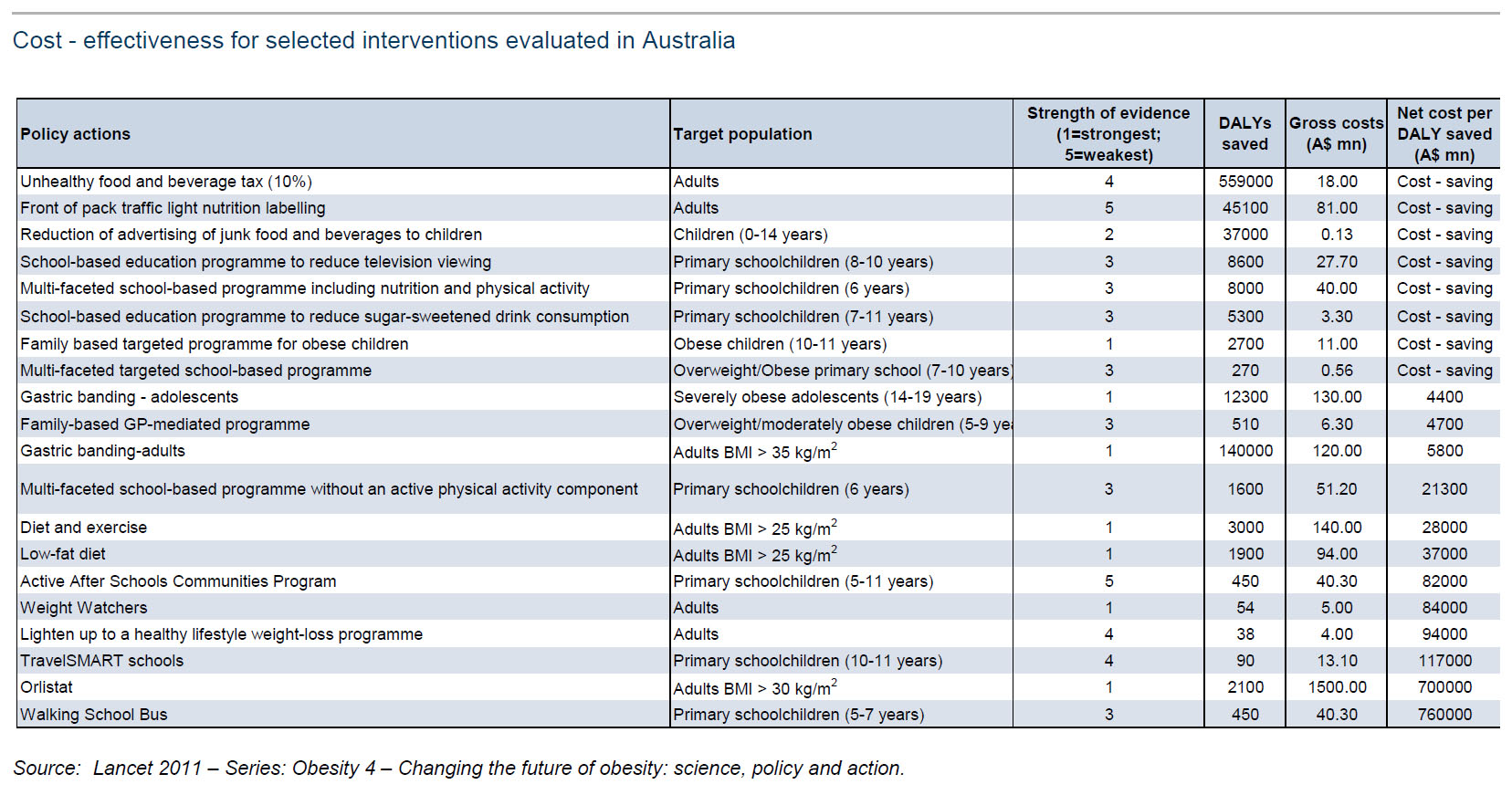
One of the more serious efforts to this end was recently demonstrated by the Australian government, which evaluated several measures aimed at combating this epidemic (see exhibit below). Not surprisingly, nonpharmacological options were found to be more cost-effective in the long term, but are obviously more difficult to implement at a society level.
* * *
Another, even more dramatic health-related recent intervention was that on behalf of Mike Bloomberg and the city of New York banning sugary drinks in 16 oz containers or more.
The problem with government intervention in individual and social level consumption, is that it never works without a proper incentive system. If instead of using negative reinforcement, the government were to use positive reinforcement techniques, and for example offer each American $100/year for every pound kept below the overweight threshold every year, the results would be far more encouraging, and the costs saved in the long run would more than offset initial outlays.
Of course, this being the government, it is absolutely certain that corruption and “unintended side-effects” will intervene, that incentives will be perverted by special interests and lobby groups, and the final outcome would be a far worse one than the base case.
Which is why, sadly, the obesity epidemic will not be “fixed” in any conventional sense, but like so many other aspects of the current unsustainable socio-economic system, will merely go away on its own once the “weakest links” are eliminated by the various forces of natural (and man-made) selection in play today.